Abstract
Background: Oncohematological patients may have a lower immune response against SARS-CoV-2, both to natural infection and to vaccines. Most studies have focused on the analysis of the humoral response, which means that the information available on the cellular response against SARS-CoV-2 in these patients is limited. Current recommendations include vaccination against SARS-CoV-2 in patients undergoing autologous hematopoietic stem cell transplantation (AHSTC), regardless of whether they have been previously exposed to the virus. These recommendations are based on previous studies with other vaccines. Therefore, it is necessary to analyze the immune response that is developed in these patients in order to make specific recommendations for COVID-19 vaccination.
Objective: To study the humoral and cellular immune response before and after AHSTC in patients with oncohematological neoplasms who were exposed to SARS-CoV-2 before the transplantation.
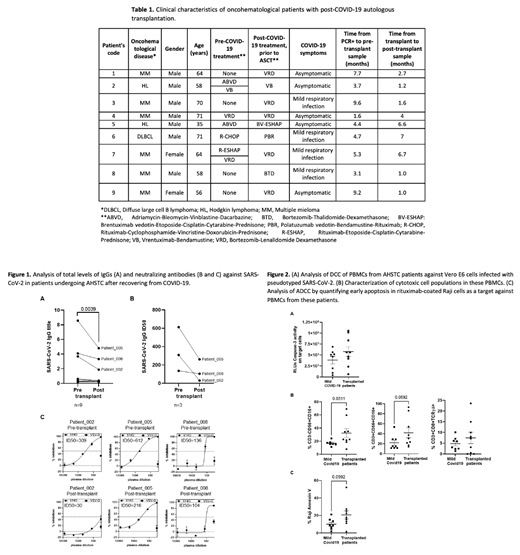
Materials & methods: Nine patients with previous exposure to SARS-CoV-2 who underwent AHSTC (Table 1) and 8 healthy donors who recovered from mild COVID-19 were recruited from Hospital Ramón y Cajal and Primary Healthcare Center Pedro Laín Entralgo (Madrid, Spain), respectively. Specific direct cellular cytotoxicity (DCC) of PBMCs from these patients against Vero E6 cells infected with pseudotyped SARS-CoV-2 was determined. The activation of caspase-3 in Vero cells was measured after 1 hour of co-culture with PBMCs, in which cytotoxic cell populations were analyzed by flow cytometry. Antibody-dependent cellular cytotoxicity (ADCC) was analyzed by quantifying the binding of Annexin V to rituximab-coated Raji cells as targets of PBMCs.
Results: 1) 66% of AHSTC patients did not develop detectable levels of IgGs against SARS-CoV-2 (Fig. 1). In 33% of these patients with detectable IgG, the titers decreased after AHSTC, as well as their neutralizing capacity (Fig. 1B and C). 2) AHSTC patients showed increased levels of immature B cells (9.5-fold; p=0.0586) and plasmablasts (28.8-fold), in comparison with healthy donors who had mild COVID-19, while naive and resting memory B cells decreased 1.7- and 6.9-fold, respectively. 3) Specific DCC against SARS-CoV-2-infected cells increased 1.5-fold in comparison with healthy donors (Fig. 2A). Cytotoxic populations with NK phenotypes (CD3-CD56+CD16+), NKT (CD3+CD56+CD16+), and CD8+ T cells (CD3+CD8+TCRγδ+) increased 1.9- (p=0.0311), 1.9- (p=0.0592), and 1.6-fold, respectively (Fig. 2B). ADCC increased 2.1-fold in PBMCs from AHSTC patients in comparison with healthy donors (p = 0.0592).
Conclusions: Our data show for the first time how the humoral and cellular immune response against the natural infection by SARS-Cov-2 may be modified in patients who were subsequently subjected to AHSTC. Although the humoral response may be reduced after AHSTC, the specific cellular response showed an increased cytotoxic activity. These results could be extrapolated to patients who were vaccinated against COVID-19 prior to AHSTC. Therefore, this information could be useful to define the recommendations for COVID-19 vaccination after AHSTC.
Garcia-Gutiérrez: Pfizer: Research Funding; Incyte: Consultancy; Novartis: Consultancy; Bristol-Myers Squibb: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal